Intrusion of the buccal segment - Palatal or Buccal Miniscrews?
Ortho Times
2 min read
General Considerations:
The mid-anterior palate has the lowest documented failure rate at 1.3%, whereas paramedian placement has a higher failure rate of 4.8% (Mohammed et al., 2018).
Palatal Miniscrews had higher survival rates than buccal (Arqub et al)
Success rates differ in relation to the anatomical site of placement (•Mohammed et al,2018)
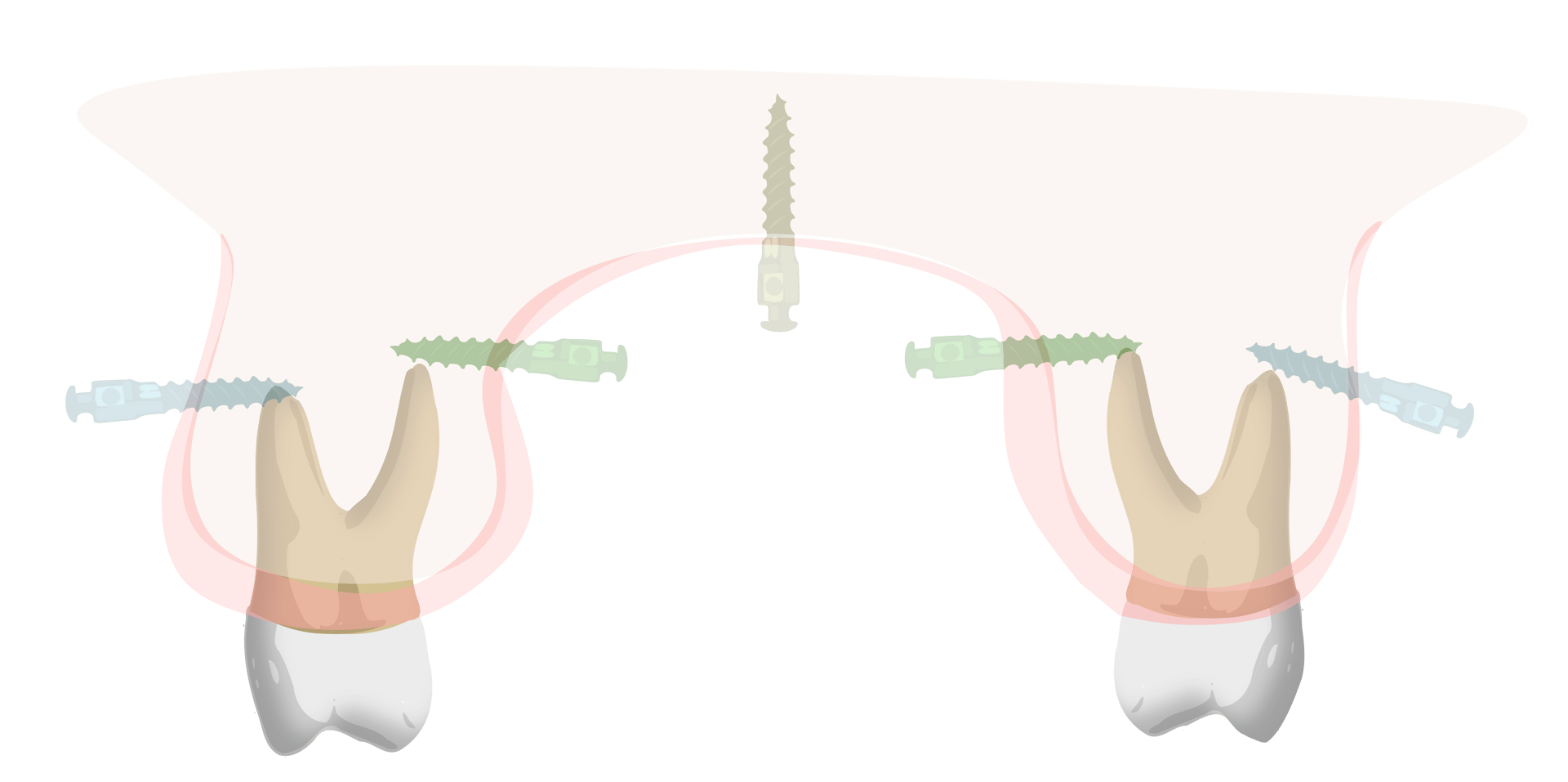
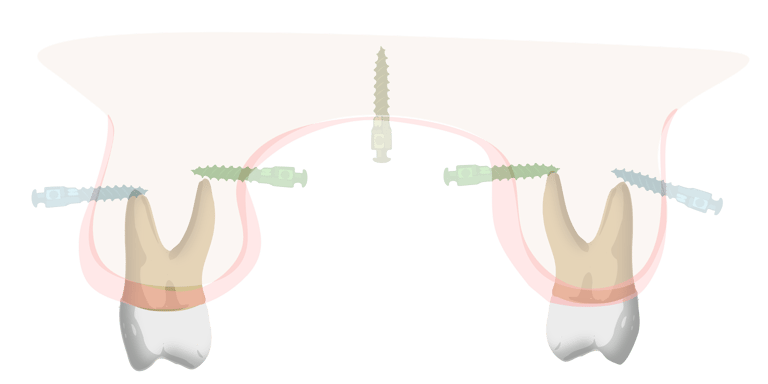
Proximity to roots and bone quality Considerations:
The risk of root injury from palatal mini-implants is minimal, especially when placed in the mid-palate, where root trauma is entirely avoided (Tae Woo Kim)
The palatal alveolar cortex is thicker compared to the corresponding buccal side, and the interproximal space between palatal roots is greater (Cousley).
In the maxilla, the greatest amount of mesiodistal bone was on the palatal side between the second premolar and the first molar. (Paola Maria Poggio , Cristina Incorvati, Stefano Velo, Aldo Carano)
Height of the miniscrew Consideration:
The TAD should be positioned sufficiently high to generate an intruding force with an extended range of action. However, the buccal attached gingiva in the region of the maxillary first and second molars is often too narrow to allow for high placement. Tae Kim Woo recommended using a single mid-palatal TAD combined with a TPA, as this provides a longer lever arm and is a more cost-effective option.
Mandibular plane angle:
Patients with a high MMPA typically have thinner buccal cortical bone compared to those with an average MMPA, resulting in a higher failure rate of maxillary buccal mini-implants in these individuals (Antoszewska et al., 2009; Moon et al., 2010).
References
Role of anatomical sites and correlated risk factors on the survival of orthodontic
miniscrew implants: a systematic review
and meta-analysis
Survival estimates and risk factors for failure of palatal and buccal mini-implants
Molar intrusion in the management of anterior openbite and ‘high angle’ Class II malocclusions
Open-Bite Correction Using a Mid-Palatal TAD with an Intrusion TPA: Anteroposterior Position of TAD
"Safe zones": a guide for miniscrew positioning in the maxillary and mandibular arch
Hygiene Considerations:
While there is no definitive consensus in the literature regarding which location is universally easier to clean, buccal miniscrews may seem the more logical choice in terms of hygiene
Gingival thickness Considerations:
The characteristics of palatal gingiva, similar to bone quality and quantity, play a role in the success of miniscrews, Thinner attached gingiva is preferred for optimal screw placement (Björn Ludwig).
Generally Palatal mucosa is thicker than Buccal mucosa.
Buccal soft tissue is thickest near and farthest from the cementoenamel junction (CEJ), with the thinnest area in the middle.
In contrast, palatal soft-tissue thickness gradually increases from the CEJ toward the apical region. (Hee-Jin Kim).
While the mucosa surrounding the lateral aspects of the palatal arch is relatively thick, it maintains a consistent thickness of only 1–4 mm at the midpalatal suture, distal to the incisive foramen (Björn Ludwig).